US Healthcare & Data Analytics Training: Benefits, Skills & Career Opportunities
-Shubham Belbase
Date: 2025-12-26
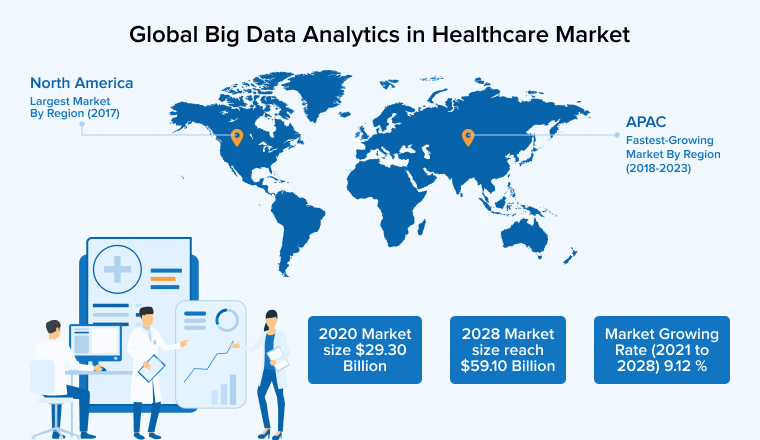
The U.S. healthcare system generates an enormous amount of data every day, and one of the most valuable sources of this information is insurance claims data. U.S. Healthcare Data Analytics, particularly in the context of claims data analytics, focuses on analyzing this data to support insurance companies in understanding costs, utilization patterns, and overall healthcare performance.
For insurance companies, this data is critical for tracking expenditures, managing risk, identifying trends, and ensuring accurate reimbursement. Given the massive valuation of the U.S. insurance market—estimated at over USD 1 trillion annually—and the rapid growth of the insurance analytics market, valued in the multi‑billion‑dollar range and growing at a strong pace, the value of insurance data itself is equally significant, making claims data analytics not just important, but indispensable.
Healthcare claims data analytics transforms this complex data into high-level, actionable insights that are easier to interpret and use. With the introduction of the Transparency in Coverage (TiC) rule, payers are now required to publish Machine-Readable Files (MRF) at scale, creating a vast and rapidly expanding data ecosystem. These insights are typically presented through graphical representations such as dashboards, charts, and trend visualizations.
Fundamental US Healthcare and Data Analytics is an 80-hour program designed to bridge the gap between US healthcare domain knowledge and technical data engineering, spanning two months of daily theory and practical sessions. The curriculum begins by grounding students in the core components of the US healthcare system, specifically focusing on the structure and analysis of critical data files, including Eligibility, Medical Claims, Pharmacy, and Provider data. It further explores complex regulatory frameworks like Machine Readable Files (MRF) and benefit logic such as deductibles, coinsurance, and out-of-pocket costs, ensuring students understand the business context behind the data.
From a technical perspective, healthcare claims and MRF data analytics rely on a modern data stack that supports large-scale processing and cloud-based analysis. Tools such as SQL and PySpark are used to manage and process high volumes of claims data, enabling the calculation of industry-standard metrics. Strong emphasis on Data Quality and cloud platforms like AWS (S3, Athena, Glue) ensures that insights are reliable, scalable, and delivered efficiently, aligning technical execution with the high-level, visual insights insurers depend on for decision-making.
Benefits:
- Enhanced Career Prospects: Gain practical skills in claims and MRF data analytics through use of dummy data for better insights to work data. This course helps learners become highly marketable in healthcare data roles such as Data Analyst, Data Quality Control(QC), ETL Engineering etc. opening doors to positions in insurance analytics, healthcare consulting, and data-driven decision-making teams.
- Hands-On Technical Expertise: Learn to use SQL, PySpark, and AWS tools for handling real healthcare data. Participants will practice processing large datasets, writing queries, and implementing analytics pipelines, ensuring they can tackle real-world challenges in a professional setting.
- Comprehensive Domain Knowledge: Understand U.S. healthcare systems, rules, and claims data. Learners gain insight into healthcare operations, regulatory frameworks, and business logic, which helps them contextualize data and communicate insights effectively with stakeholders.
- Competitive Edge: Build a strong skill set to analyze complex healthcare data and stand out in the insurance analytics market. Graduates will have the confidence and expertise to handle large-scale datasets, provide strategic recommendations, and advance in a rapidly growing, high-value industry.
- Interaction with Experienced Trainers: Connect with trainers who have worked in the healthcare analytics field for multiple years. This allows trainees to gain practical insights, learn industry best practices, and receive mentorship that bridges theory with real-world application.
Career Opportunities:
Graduates can explore career opportunities in Nepal with multiple big companies such as Cedar Gate, Deerhold, Maitri Services, Verisk, Infinite,Codavatar and many more. These roles include positions in Data analytics, healthcare analytics, data quality, ETL engineering, Quality Control(QC) and Quality Assurance allowing trainees to apply technical skills and domain knowledge gained in the course. With the growing demand for healthcare data expertise, participants can also expect exposure to projects involving large-scale claims and MRF datasets, dashboards, and reporting, providing a strong foundation for long-term career growth in the Nepalese market and potential opportunities abroad.